New York, Dec 3 (IANS) Researchers have found that a protein involved in immune response to microbes also can fuel cancer development and suppress the response to the disease.
Working in mouse models of lung cancer, the research team found TANK-binding kinase 1 (TBK1) and its adaptor proteiTBK-binding protein 1 (TBKBP1) contribute to tumorigenesis when they are activated by growth factors rather than by innate immune mechanisms.
“Our work also provides the first evidence that TBK1 functions in cancer cells to mediate immunosuppression, suggesting that targeting TBK1 will both inhibit tumour growth and promote antitumor immunity,” said study senior author Shao-Cong Sun from University of Texas in the US.
Recent research indicated that TBK1, which normally mediates induction of type 1 interferon in response to viruses or bacteria, also promotes the survival and reproduction of KRAS-dependent cancer cells.
For the findings published in the journal Nature Cell Biology, the research team set out to identify TBK1’s impact on cancer cells and its role in cancer development in vivo.
In a series of experiments, the researchers showed that TBK1 and TBKBP1 form a growth factor signaling axis that activates mTORC1 to promote tumour development.
The pathway consists of TBKBP1 recruiting TBK1 to protein kinase C-theta (PKC), through a scaffold protein called CARD10, enabling PKC to activate TBK1.
To test the protein’s therapeutic potential, the research team treated mice with KRAS-driven lung cancer with amlexanox, a drug approved by the Food and Drug Administration as a paste to treat certain oral ulcers.
The drug was recently identified as a TBK1 inhibitor. Mice injected with amlexanox had a steep reduction in the number and size of lung tumors.
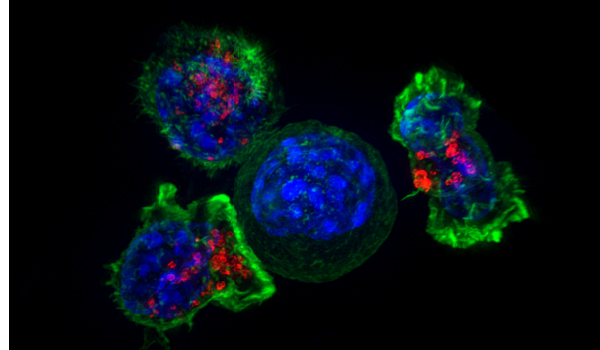
KRAS-driven cancer is resistant to immune response, but the researchers found amlexanox sensitised tumours to blockade of the CTLA-4 checkpoint on immune T cells.
Knocking down TBK1 in the KRAS-driven mouse model increased the frequency of effector CD4 helper T cells and CD8 cell-killing T cells in the lungs of the mice.
A similar experiment in another mouse model also reduced the frequency of immune-suppressing myeloid-derived suppressor cells.
Additional experiments implicated TBK1 in promotion of glycolysis – a sugar-burning metabolic process that also suppresses the immune system – and the increased presence of PD-L1, a protein on tumour cells that turns off attacking T cells by connecting with the PD-1 protein on their cell surface.
Treatment with amlexanox and anti-CTLA-4 immunotherapy stimulated immune response and reduced tumour size and frequency in the mouse models.
“We’re continuing to examine the signaling function of TBK1 in different types of immune cells using animal models and to assess the therapeutic potential of TBK1 using preclinical cancer models,” Sun said.